A short disclaimer first
I’m not a doctor or an autism expert. I’m just a dad trying to make sense of why my son has struggled to learn and develop, especially verbally.
Everything I share here reflects my own views and experiences unless I reference external sources.
Every child with autism has their own unique story. This blog focuses on Adam’s story so far.
My hope is that by sharing ours, it may help you begin stitching together your own. And maybe, together, we can all learn from our experiences to better support our children.
The Beginning: Adam’s Arrival and the First Set of Clues
Adam was born in the winter of 2021 via C-section. At the time I didn’t think twice about it. Later, I learned how a C-section can influence a baby’s microbiome and immune system, particularly because the mother’s beneficial bacteria are not transferred in the same way.
Breastfeeding lasted only two weeks due to complications, and Adam moved onto formula. We started with Aptamil, which caused reflux, and later switched to HiPP Organic, which seemed to suit him better.
At the time, I didn’t yet understand how powerful breast milk can be for a baby’s brain, immune system, and overall development. I’ve since learned how protective it can be against infections and longer term health issues. [source]
After a few months, Adam was circumcised but developed an infection and had to be put on antibiotics. That was his first course, and unfortunately not his last. A midwife also noted he had a tongue tie, but at the time we didn’t take any action.
Life felt normal enough back then. Looking back now, I can see the clues were already there.

Before Adam Was Born: The Invisible Things That Matter
Before Adam was born, my wife had long standing hyperthyroid issue, even though her hormone tests during pregnancy always came back “normal.” She also couldn’t tolerate folic acid. Whenever she took it, her thyroid nodules grew larger. I later learned that this intolerance can sometimes point toward
methylation issues
Methylation is a vital biochemical process that occurs in every
cell of the body. It acts like a series of tiny switches that help regulate
gene expression, detoxification, and the production of brain chemicals
such as neurotransmitters.
Some research suggests that children with autism may have impaired
methylation, which could affect brain development, detox pathways,
and the body’s ability to produce important antioxidants like glutathione.
Because of this, some practitioners explore targeted nutritional support,
such as methylated B vitamins or folate, to help support these pathways.
Research reference: James et al., American Journal of Clinical Nutrition (2009)
, such as MTHFR.
She also had dental issues for several years, including during pregnancy, and had mercury amalgam fillings. These weren’t addressed until much later.
There had also been a miscarriage shortly before Adam was conceived.
At the time, none of this felt connected. Today, it feels relevant enough to include as part of the bigger picture.
Year One: Gut Problems and Ear Problems Become a Theme
By the end of Adam’s first year, we were already dealing with more than we realised:
- glue ear
- chronic sinus issues
- noisy breathing during sleep
- multiple suspected infections
- several rounds of antibiotics
- frequent loose stools
- gas and bloating
Adam occasionally responded to his name and sometimes gave eye contact. He vocalised constantly, making sounds and noises, but actual words were rare.
Physically, he was strong. He walked at around fourteen months and climbed everything he could. But something inside his body didn’t seem comfortable. His gut and ears were in constant trouble.
Year Two: The Patterns Intensify
By 2023, Adam’s loose stools increased to four or five times a day. He developed painful sores around his bottom from the constant wiping, which required antibiotic cream.
He also had surgery for a hernia and a hydrocele, something we had known about since he was a few months old. This meant hospital stay and likely another exposure to antibiotics.
Sleep became harder. Some nights he woke and couldn’t settle again. He also appeared to have a higher tolerance for pain.
At the same time, his strengths became more obvious. Adam was a great imitator. He copied cooking, ironing, and cleaning. He pushed his toy ice cream trolley around the house doing his own make believe play. He rode his push car, sometimes at great speeds. He followed lines on the floor. He even worked out that he could throw my boxing glove at a cupboard door until it opened. His pretend play was genuinely funny and creative.
Speech didn’t come, but understanding was clearly there.
And this was also when a very puzzling behaviour became more noticeable.
The Goofy Giddy “Almost Drunk” Episodes
From around age two, Adam would sometimes shift into a strange state. He would laugh uncontrollably, become overly silly, impulsive, hyper, and very difficult to regulate. These episodes could last anywhere from ten to thirty minutes.
Sometimes they happened after eating, especially sugary or carbohydrate-heavy foods like biscuits, cereal bars, cakes or rice. Other times, they happened purely from excitement, particularly when he saw me. That distinction became important later.
It wasn’t always food triggered, but food often intensified it.
At first, we thought this was just sensory excitement. But over time, I couldn’t ignore how often these episodes followed certain foods. It felt like something biochemical was going on.

I didn’t know the term at the time, but what we were seeing resembled what some
functional medicine
Functional medicine is an approach to healthcare that focuses
on understanding and addressing the root causes of health problems,
rather than simply treating symptoms.
In the context of autism, functional medicine practitioners often explore
underlying factors such as gut health, nutritional deficiencies,
immune system regulation, and environmental or toxic exposures that may
be contributing to a child’s symptoms.
This approach emphasises personalised support, with interventions tailored
to each child’s unique biology and needs.
Research reference: Frye & Rossignol,
Frontiers in Pediatrics (2014)
practitioners describe as fermentation spikes or an “auto brewery” type pattern,
where certain gut microbes ferment carbohydrates into alcohol like compounds.
This explanation later suddenly connected many dots, especially when we noticed that Adam’s breath sometimes smelled sulphur like while he was sleeping.
Year Three: Therapies, Small Gains, and Continuing Confusion
We tried speech therapy and occupational therapy. Adam made some progress, but not the kind of breakthroughs we were hoping for. He moved into a special needs educational setting that follows ABA principles, the structure did seem to help him.
We tried CBD oil and melatonin for about a year. The CBD helped him feel somewhat calmer, and melatonin helped him sleep.
He remained preverbal but consistently vocal. He made sounds, babbled, copied tones, and expressed himself in his own way, but words were still inconsistent.
Despite all this effort, we still didn’t have a clear explanation for what was happening inside his body.
Vaccinations and Adam’s Immune Load
Many parents will wonder about vaccinations, so I want to be open about our choices and thought process.
Adam received all standard vaccines except the combined MMR. We opted for the single measles vaccine instead. One reason for this was that I had already seen changes in my nephew after the MMR, and he was later diagnosed with autism. That experience stayed with me.
I also felt mumps was less of a concern and rubella could be addressed later if needed. Adam also received the flu vaccine and the teenage meningitis vaccines.
I’m not here to make declarations or claims. I’m still trying to understand my own position. What I do know is that Adam had a developing immune system that was already dealing with:
- antibiotics
- C-section birth
- gut issues
- chronic ENT infections
- maternal influences
- environmental load
I do believe aluminium adjuvants may contribute to the total body burden in some children more than others. There is published research suggesting aluminium can cross the blood brain barrier. [source] [source]
Because of this, I decided to try silicon rich mineral water for Adam, something discussed by Professor Chris Exley as a non invasive way to potentially help the body eliminate aluminium. Whether this is helping or not, I don’t yet know, as it’s only been around six months. But it felt like a gentle, low-risk step worth exploring.
This is simply my own reflection as a parent, not a universal claim.
Year Four: More Clarity, Some Progress and New Rigidities
IIn early 2025, Adam had his tonsils and adenoids removed after seeing an ENT specialist. The hope was that this would reduce his sinus issues and frequent winter infections. ENT also confirmed his hearing was now normal after years of glue ear.
Around the same time, we introduced daily supplements including magnesium glycinate, vitamin D3, K2, cod liver oil, zinc, and a few others. Adam refused powders but tolerated liquids well. I’ll share more about this in a future post.
A few months later, something interesting happened. His stools shifted from loose and frequent to firmer and heavier, usually once or twice a day. This could also suggest mild constipation, but it was a clear change.
Some things stabilised. Others didn’t.
He still experienced bloating.
He still had behavioural spikes after carbohydrates.
He still occasionally had sulphur smelling breath.
He still had sinus issues in winter, though less severe.
He still flushed red in his ears and cheeks when warm or overstimulated.
But there were also some small moments that mattered.
For the first time, Adam began sitting with a book, looking at the pictures, recognising a banana, and calling it out in his own way by saying “mama.” It wasn’t perfect or consistent, but it mattered. Around the same time, at his speech and language therapy just before the Christmas holidays, he also started copying the animal sounds and noises the therapist was making. This felt like a small window opening.
We’ve also noticed increased rigidity too. More resistance to changing shoes or jackets. More stimming. More OCD like patterns. His sensory world seems to be shifting again.
Progress doesn’t always move in a straight line. Some doors open quietly while others feel harder to push, but those small wins remind us that things are happening, even when the bigger picture feels uncertain.
Slowly the Picture Became Clearer
After years of observing, note taking, researching, listening to practitioners, and watching Adam closely day by day, a clearer picture began to form. It wasn’t autism alone. It wasn’t behaviour, diet, genetics, or immune load on their own. It was everything interacting.
Around the summer, something happened that helped this idea really click. While casually scrolling through YouTube, I came across a video about a boy named Reeve Anderson in the US. He had Down syndrome and experienced a sudden regression at age four, losing the ability to walk. Eventually, Dr Richard Frye identified a folate pathway issue and treated him with leucovorin, a form of vitamin B9. I was amazed that a vitamin could have such a profound effect.
That moment sent me down a rabbit hole. I read Brain Inflamed by Dr Kenneth Bock, which looks at neurodevelopment through inflammation and immune imbalance rather than psychology alone. I also came across the podcast Functional Medicine Doc Talk with Dr Kurt Woeller and later read Biological Treatments for Autism and PDD by Dr William Shaw.
I found a framework that aligned with what I had been observing in Adam for years. It didn’t give me instant answers, but it finally gave me a way to connect the dots.
The Hypothesis That Finally Made Sense
The working model
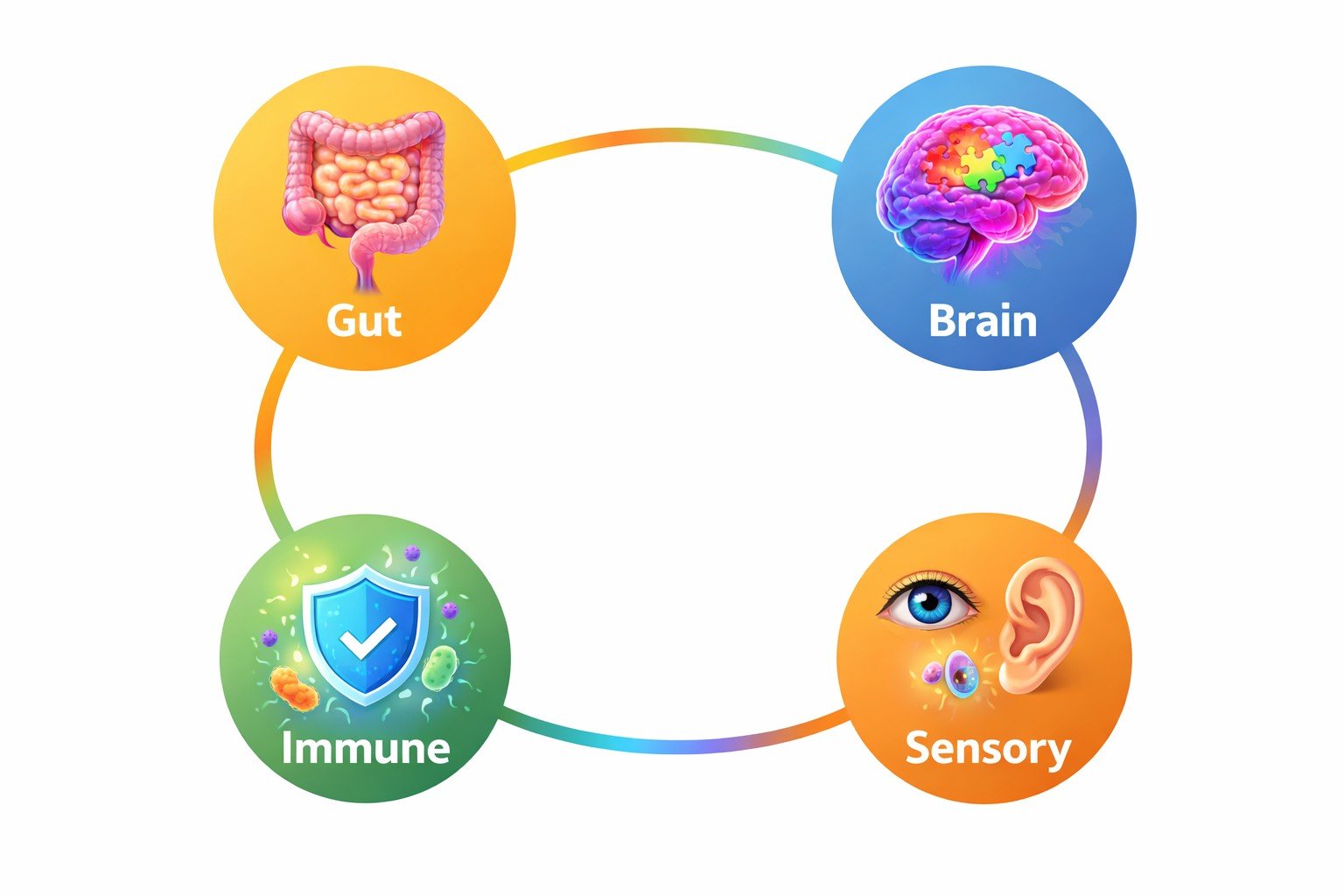
In simple terms, I began to see Adam’s challenges not as one single issue, but as multiple systems interacting: the gut, the immune system, the brain, and the sensory world.
Here’s the working hypothesis I’ve arrived at so far.
1. Gut Dysbiosis and Carbohydrate Fermentation
Adam’s early history of C-section birth, antibiotics, formula feeding, vaccinations, and chronic infections may have left him with a vulnerable gut and immune system.
Years of diarrhoea, rashes, bloating, and strong reactions to sugar pointed toward
an
imbalance in gut microbes
Gut dysbiosis is an imbalance in gut bacteria — when there are
too many “bad” microbes and not enough beneficial ones.
In children with autism, this imbalance is common and may contribute
to digestive symptoms like constipation, diarrhoea, bloating,
and stomach pain.
The gut and brain communicate through the gut–brain axis,
meaning changes in gut bacteria may also influence behaviour and regulation.
Ref: Fattorusso et al., Nutrients (2019)
,
particularly yeast or fermenting bacteria.
In these situations, carbohydrates may be broken down into by-products the body struggles to handle, potentially affecting behaviour and attention.
Some researchers also describe how ongoing gut inflammation may weaken the gut lining, sometimes referred to as “leaky gut,” allowing substances to enter the bloodstream that can trigger inflammation elsewhere, including the brain.
Not all of Adam’s behaviours come from his gut, but food clearly makes a difference.
2. Histamine and Mast Cell Sensitivity
Adam’s sinus congestion, red ears and cheeks, seasonal flares,
and response to antihistamines suggest
histamine sensitivity
Histamine sensitivity (also called histamine intolerance)
occurs when the body struggles to break down histamine properly,
leading to a buildup.
Histamine is a natural chemical found in certain foods and is also
released by the body during allergic or inflammatory responses.
In some children with autism, researchers suggest histamine
processing may be altered, potentially contributing to symptoms
such as hyperactivity, sleep disturbances, skin flushing,
digestive discomfort, or sensory overload.
Ref: Theoharides et al., Journal of Neuroinflammation (2013)
.
Certain foods, including gluten, and certain gut microbes can increase histamine, which may amplify sensory and behavioural responses.
3. Methylation Vulnerability
My wife’s folic acid intolerance, thyroid nodules, pregnancy inflammation, and dental issues point toward a possible methylation and detox vulnerability.
This could potentially help explain:
- speech delay
- sensory sensitivities
- rigidity and stimming
- histamine reactivity
- gut permeability
- inflammation
This feels like a significant piece of the puzzle.
4. Sensory and Emotional Overflow
Adam seems to experience two types of silly behaviour:
- metabolically driven episodes
- excitement driven episodes
Seeing me can trigger a silly spiral even without food. That feels more like sensory seeking and emotional overflow. Food probably doesn’t create this neurology, but it often makes it harder for him to regulate.
5. Speech Delay Linked to Early ENT & Gut-Brain Axis
Years of glue ear and infections likely affected how Adam heard and processed speech during critical developmental windows.
His strong imitation and pretend play show understanding and intelligence. His expressive language hasn’t caught up yet.
His speech delay feels neurological, sensory, and metabolic all at once.
Why I’m Sharing All of This
Because we question ourselves, and sometimes worry we’re imagining patterns.
Because professionals often see only one part of the picture,
while our children live in the whole picture.
If you are seeing things like
- bloating
- loose stools
- carb cravings
- goofy episodes
- red ears or cheeks
- sinus issues
- rigidity
- speech delays
- sulphur breath
- reactions to sugar or gluten
- big highs and lows
- skin sensitivities
- inconsistent language
- higher pain tolerance
Your child may also have a gut-immune-brain story. Not identical to Adam’s, but similar enough that connecting these dots might help you understand what your child is showing you.
We are still on this journey, still learning, still trying, still piecing things together. But this is the clearest picture we’ve had so far, and it’s helped us see Adam as a whole child whose systems are deeply connected.
I don’t believe this is simply a fixed neurological issue where nothing can change. I believe there is more going on beneath the surface. And if sharing Adam’s story gives even one parent an “aha” moment, then it’s worth telling.
The next step for us is to look a little deeper. We’re now planning to explore targeted testing, guided by a functional medicine doctor, to see what Adam’s biology might be telling us. Whatever comes back, we’ll take things slowly, thoughtfully, and with support.
Thank you for reading, until next time, may God bless you.
Zee
test